Bone marrow is the spongy tissue inside some of the bones in the body, including the hip and thigh bones. Bone marrow contains immature cells, called stem cells.
Numerous people with blood cancers such as leukemia, lymphoma, sickle cell anemia and other life-threatening diseases, rely on bone marrow or cord blood transplants to save their life.
Healthy bone marrow and blood cells are needed in order to live. When disease affects bone marrow so that it can no longer function effectively, a marrow or cord blood transplant could be the best treatment option, and for some patients, it offers the only potential cure.
Contents of this article:
- What is bone marrow?
- What does bone marrow do for your body?
- What are bone marrow tests?
- What is a bone marrow transplant?
- Reasons for bone marrow transplants
- Diagnosis and preparation
- How is bone marrow harvested?
- How does a bone marrow transplant occur?
- What are the risks of bone marrow transplants?
- What is bone marrow donation?
- What happens when donating bone marrow?
- Outcomes
Fast facts on bone marrow
Here are some key points about bone marrow. More detail and supporting information is in the main article.
- A bone marrow transplant can save the lives of people battling leukemia, lymphoma and other blood cancers.
- At birth, all bone marrow is red. As humans age, red marrow increasingly begins to convert to yellow marrow.
- In adults, around half of the bone marrow is red and half is yellow.
- 200 billion new blood cells are made by the bone marrow every day.
- Healthy bone marrow manufactures between 150,000 and 450,000 platelets per microliter of blood, the amount of blood that fits on the head of a pin.
- Bone marrow contains mesenchymal and hematopoietic stem cells.
- Around 10,000 people in the US are diagnosed each year with diseases that require bone marrow transplants.
- 7 out of 10 people who require a bone marrow transplant do not have a matching donor in their family, and rely on the registry of bone marrow donors to find a match.
- The process for matching a patient with a donor involves comparing human leukocyte antigen (HLA) types in order to find a match.
- Several diseases, often incurable, pose a threat to bone marrow and prevent bone marrow from turning stem cells into essential cells.
What is bone marrow?
Bone marrow is soft, gelatinous tissue that fills the medullary cavities - the centers of bones. There are two types of bone marrow: red bone marrow (also known as myeloid tissue) and yellow bone marrow (fatty tissue).1
Both types of bone marrow are highly vascular and enriched with numerous blood vessels and capillaries.2
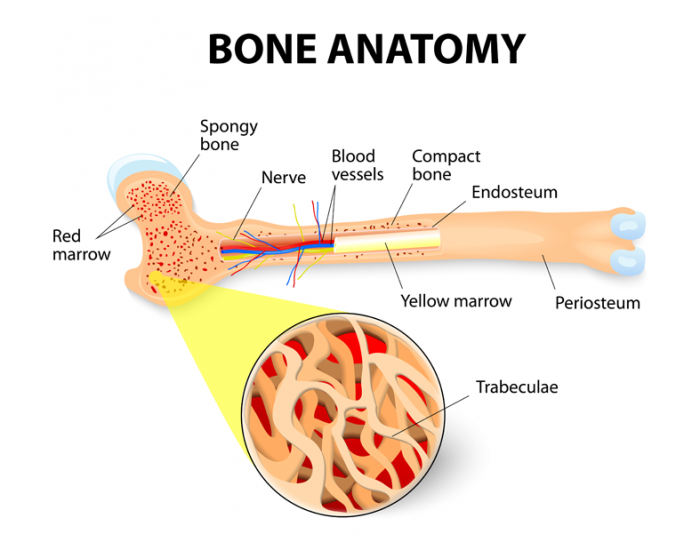
Long bone cross-section showing both red and yellow bone marrow.
The bone marrow makes more than 200 billion new blood cells every day.8 Most blood cells in the body develop from cells in the bone marrow.5
Stem cells
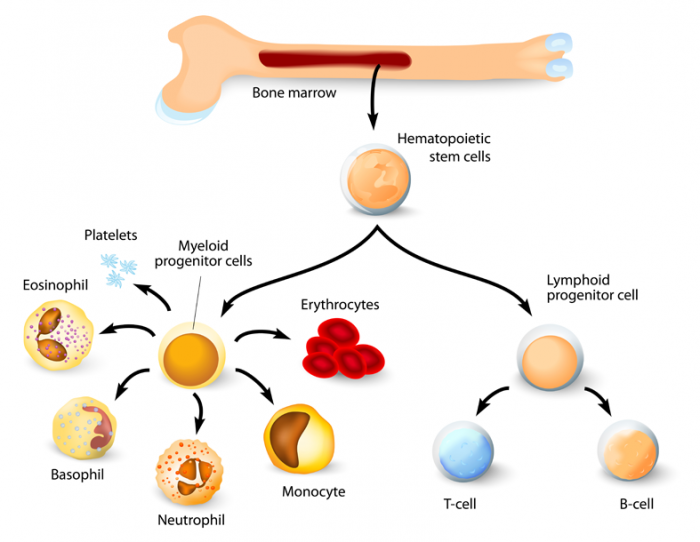
The bone marrow has two types of stem cells: mesenchymal and hematopoietic.
Red bone marrow consists of a delicate, highly vascular fibrous tissue containing hematopoietic stem cells, which are blood-forming stem cells.
Yellow bone marrow contains mesenchymal stem cells, also known as marrow stromal cells, which produce fat, cartilage and bone.4
Stem cells are immature (primitive) cells. There are two main types in the bone marrow that hematopoietic stem cells give rise to - myeloid and lymphoid lineages. These derive from even more primitive cells called common pluripotent stem cells.
The most primitive of the stem cells is called the pluripotent stem cell, which is different from other blood cells due to the following properties:
- Renewal: can reproduce another cell identical to itself
- Differentiation: can generate one or more subsets of more mature cells.
The process of development of different blood cells from these pluripotent stem cells is known as hematopoiesis.11
It is these stem cells that are needed in bone marrow transplant.
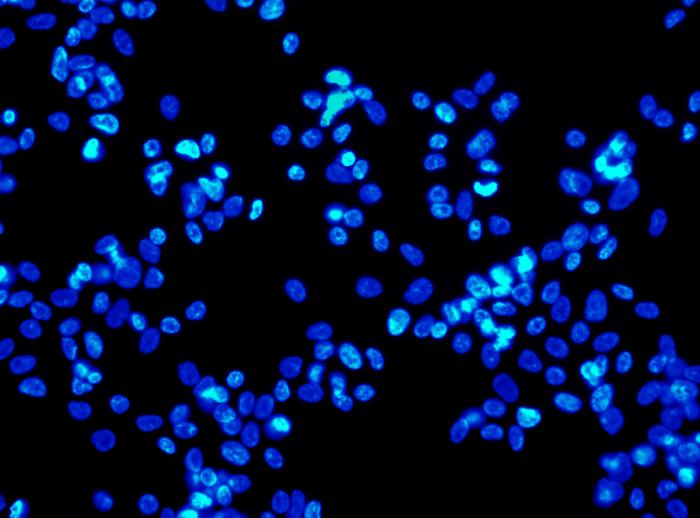
Stem cells constantly divide and produce new cells. Some new cells remain as stem cells and others go through a series of maturing stages (precursor or blast cells) before forming into fully formed (mature) blood cells. Stem cells rapidly multiply to make millions of blood cells each day.10
Blood cells have a limited life span and are constantly being replaced. The production of healthy stem cells is vital.12
The blood vessels constitute a barrier, inhibiting immature blood cells from leaving the bone marrow. Only mature blood cells contain the membrane proteins required to attach to and pass the blood vessel endothelium. Hematopoietic stem cells may also cross the bone marrow barrier, and may be harvested from blood.15
The blood-forming stem cells in red bone marrow can multiply and mature into three significant types of blood cells, each with their own job:
- Red blood cells (erythrocytes) - transport oxygen around the body
- White blood cells (leukocytes) - help fight infection and disease. White blood cells include lymphocytes - the cornerstone of the immune system - and myeloid cells which include granulocytes: neutrophils, monocytes, eosinophils, and basophils
- Platelets (thrombocytes) - aid with clotting after injury. Platelets are fragments of the cytoplasm of megakaryocytes, another bone marrow cell.
Once mature, these blood cells migrate from the marrow and are introduced into the bloodstream, where they provide important functions in keeping the body alive and healthy.7
Mesenchymal stem cells are found in the bone marrow cavity and differentiate into a number of stromal lineages, such as chondrocytes (cartilage generation), osteoblasts (bone formation), osteoclasts, adipocytes (adipose tissue), myocytes (muscle), macrophages, endothelial cells and fibroblasts.6
Red bone marrow
All blood cells in humans are formed in the red bone marrow, with the exception of lymphocytes, which are formed in the marrow but reach maturity in the lymphoid organs.1
Red bone marrow also plays a role in the obliteration of old red blood cells, along with the liver and spleen.
Yellow bone marrow
Yellow bone marrow's main purpose is to act as a store for fats and serves to provide sustenance and maintain the correct environment for the bone to function. However, under particular conditions, such as severe blood loss or fever, the yellow may revert to red marrow.1
Yellow marrow tends to be located in the center-most cavities of long bones, and is generally surrounded by a layer of red marrow with long trabeculae (beam-like structures) within a sponge-like reticular framework.6
Bone marrow timeline
Bone marrow first occurs in the clavicle near the end of fetal life and becomes active about 3 weeks later. Bone marrow supersedes the liver as the major hematopoietic organ at 32-36 weeks' gestation.
Bone marrow remains red until around the age of seven as the need for new continuous blood formation is high. As the body ages, the red marrow is gradually replaced by yellow fat tissue. Adults have on average about 2.6kg (5.7lbs) of bone marrow, with about half of it being red.3
In adults, red marrow has its strongest concentrations in the bones of the vertebrae, hips (ilium), breastbone (sternum), ribs, skull and at the metaphyseal and epiphyseal ends of the long bones of the arm (humerus) and leg (femur and tibia). All other cancellous, or spongy, bones and central cavities of the long bones are filled with yellow marrow.
What does bone marrow do for your body?
The majority of red blood cells, platelets, and most of the white blood cells are formed in the red marrow while only a few of them are formed in the yellow marrow.
White blood cells survive anywhere from a few hours to a few days, platelets for about 10 days, and red blood cells for about 120 days. These cells must be constantly replaced by the bone marrow as each blood cell has a set life expectancy. Certain conditions may trigger additional production of blood cells.
When the oxygen content of body tissues is low, if there is loss of blood or anemia, or if the number of red blood cells decreases, the kidneys produce and release erythropoietin, a hormone that stimulates the bone marrow to produce more red blood cells.
Similarly, the bone marrow produces and releases more white blood cells in response to infections, and more platelets in response to bleeding. If a person experiences serious blood loss, yellow bone marrow can be activated and transformed into red bone marrow.
Bone marrow's function is important for:
Blood cell formation from differentiation of hematopoietic stem cells in red bone marrow.
Circulatory system
The circulatory system touches every organ and system in the body. Red cells are carried in the circulation of blood to transport oxygen.
Hemoglobin
Hemoglobin protein is found within red blood cells and gives them their color.
Hemoglobin collects oxygen in the lungs, transports it in the red blood cells, and releases oxygen to tissues such as the heart, muscles, and brain. CO2 waste product is also removed by hemoglobin and sent back to the lungs where it is exhaled.
Iron
Iron is an important nutrient within the body. It combines with protein to make the hemoglobin in red blood cells and is essential in the production of red blood cells (erythropoiesis). The body stores iron in the liver, spleen, and bone marrow. Most of the iron needed each day for making hemoglobin comes from the recycling of old red blood cells.
Red blood cells
The production of red blood cells is called erythropoiesis. It takes about 7 days for a committed stem cell to mature into a fully functional red blood cell. As red blood cells age, they become less active and become more fragile.
Aging red cells are removed or eaten up by white blood cells (macrophages) in a process known as phagocytosis and the contents of these cells are released into the blood. The blood stream carries the iron from the hemoglobin of the destroyed cells to either the bone marrow for production of new red blood cells or to the liver or other tissues for storage.
Normally, around 1% of the body's total red blood cells are replaced every day. The number of red blood cells produced each day, in a healthy person, is about 200 billion cells.
White blood cells
The bone marrow produces many types of white blood cells, which are necessary for a healthy immune system. These cells both prevent and fight infections.
The main types of white blood cell or leukocytes are:
Lymphocytes
Lymphocytes are produced in bone marrow. They make natural antibodies to fight infection caused by viruses that enter the body through the nose, mouth, or cuts and grazes. This takes place through recognizing foreign substances that enter the body and then sending a signal to other cells to attack them. The number of lymphocytes increases in response to these invasions. There are two major types - B- and T-lymphocytes.
Monocytes
Monocytes are also produced in the bone marrow. Mature monocytes have a life expectancy in the blood of only 3-8 hours, but when they move into the tissues, they mature into larger cells called macrophages. Macrophages can survive in the tissues for long periods of time where they engulf and destroy bacteria, some fungi, dead cells, and other material foreign to the body.
Granulocytes
Granulocyte is the family or collective name given to three types of white blood cells: neutrophils, eosinophils and basophils. The development of a granulocyte may take two weeks, but this time is shortened when there is an increased threat like a bacterial infection.
The bone marrow also stores a large reserve of mature granulocytes. For every granulocyte circulating within the blood, there may be 50-100 cells waiting in the marrow to be released into the blood stream. As a result, half the granulocytes in the blood stream can be available to actively fight an infection in the body within 7 hours of recognizing that an infection exists. Once a granulocyte has left the blood it does not return.
A granulocyte may survive in the tissues for as long as 4-5 days depending on the conditions, but it only survives for a few hours in the circulation.
Neutrophils
Neutrophils are the most common granulocyte. They can attack and destroy bacteria and viruses.
Eosinophils
Eosinophils are involved in the fight against many types of parasitic infections and against the larvae of parasitic worms and other organisms. They are also involved in some allergic reactions.
Basophils
Basophils are the least common of the white blood cells and respond to various allergens that cause the release of histamines and other substances.
These substances cause irritation and inflammation in the affected tissues.
The human body recognizes the irritation or inflammation and dilates the blood vessels allowing fluid to leave the circulatory system and enter the tissue in an effort to dilute the irritant. This reaction is seen in hay fever, some forms of asthma, hives, and in its most serious form, anaphylactic shock.
Platelets
Platelets are produced in bone marrow by a process known as thrombopoiesis. Platelets are critical to blood coagulation and the formation of clots to stop bleeding.
Sudden blood loss triggers platelet activity at the site of an injury or wound. Here, the platelets clump together and combine with other substances to form fibrin. Fibrin has a thread-like structure and forms an external scab or clot.
Platelet deficiency causes the body to bruise and bleed more easily. Blood may not clot well at an open wound, and there may be a greater risk for internal bleeding if the platelet count is very low.
Lymphatic system
The lymphatic system is made up of lymphatic organs such as bone marrow, the tonsils, the thymus, the spleen and lymph nodes.
All lymphocytes develop in the bone marrow from immature cells called stem cells. Lymphocytes that mature in the thymus gland (behind the breastbone) are called T-cells. Lymphocytes that mature in the bone marrow or lymphatic organs are called B-cells.14
Immune system
Our immune system protects the body from disease. It kills unwanted micro-organisms such as bacteria and viruses that may invade our bodies.
How does our immune system fight against infection?
Small glands called lymph nodes are scattered throughout the body. Once made inside our marrow, lymphocytes enter the lymph nodes. The lymphocytes travel between each node through channels called lymphatics. The lymphatic channels meet at large ducts that empty into a blood vessel. Lymphocytes enter the blood through these ducts.
There are three major types of lymphocytes, which play an important part of the immune system:
There are three types lymphocytes. T-lymphocytes, B-lymphocytes and natural killer cells.
B-lymphocytes (B-cells)
These cells originate in the bone marrow. They make proteins called antibodies which attach onto the surface of infection-causing microbes. These are Y or T-shaped.
Each antibody reacts to different microbes by sticking to molecules called antigens, which sit on the surface of the microbe. It is this antibody-antigen binding that triggers B-cells to grow and produce more antibodies which fight infection.
T-lymphocytes (T-cells)
These cells mature in the thymus, a small organ in the upper chest, just behind the sternum. T-cells help B-cells make antibodies against invading bacteria, viruses, or other microbes. Unlike B-cells, T-cells engulf and destroy pathogens directly, after binding to the antigen on the surface of the microbe.
Natural killer (NK) cells
These are a type of lymphocyte that directly attacks cells which have been infected by a virus.
What are bone marrow tests?
Examination of the bone marrow is helpful in diagnosing certain diseases, especially those related to blood and blood-forming organs. Testing provides information on iron stores and blood production.1
Bone marrow aspiration (the removal of a small sample of bone marrow through a needle for examination under a microscope) of a small amount (about 1 ml) of bone marrow is accomplished by suction through a hollow needle. The needle is usually inserted into the hip or sternum in adults and into the upper part of the tibia (the larger bone of the lower leg) in children.
The necessity for a bone marrow aspiration is ordinarily based on previous blood studies and is particularly useful in providing information on various stages of immature blood cells.
Disorders in which bone marrow examination is of special diagnostic value include:1
- Leukemia
- Multiple myeloma
- Gaucher disease
- Unusual cases of anemia
- Other hematological diseases.
What is a bone marrow transplant?
A bone marrow transplant can be used to:
- Replace diseased, nonfunctioning bone marrow with healthy functioning bone marrow (for conditions such as leukemia, aplastic anemia, and sickle cell anemia).
- Regenerate a new immune system that will fight existing or residual leukemia or other cancers not killed by chemotherapy or radiation.
- Replace bone marrow and restore its normal function after high doses of chemotherapy or radiation are given to treat a malignancy.
- Replace bone marrow with genetically healthy functioning bone marrow to prevent further damage from a genetic disease process (such as Hurler's syndrome and adrenoleukodystrophy).
Stem cells are located in three places - bone marrow, peripheral blood (found in blood vessels throughout the body) and cord blood (found in the umbilical cord and collected after the baby's birth). Stem cells for transplantation are obtained from any of these three places.9
Stem cells can be obtained from bone marrow, peripheral blood and cord blood.
Hematopoietic stem cell transplantation involves the intravenous infusion stem cells collected from bone marrow, peripheral blood, or umbilical cord blood to re-establish hematopoietic function in patients whose bone marrow or immune system is damaged or defective.17
More than 50,000 first hematopoietic stem cell transplantation procedures, 28,000 autologous transplantation procedures, and 21,000 allogeneic transplantation procedures are performed every year worldwide, per the first report of the Worldwide Network for Blood and Marrow Transplantation.
This number continues to increase by 10-20% annually, and reductions in organ damage, infection, and severe, acute graft versus host disease (GVHD) seem to be contributing to improved outcomes. In a study of 854 patients who had survived at least 2 years after autologous hematopoietic stem cell transplantation (HSCT) for hematologic malignancy, 68.8% were still alive 10 years after transplantation.17
A number of diseases, often incurable, pose a threat to bone marrow. They prevent bone marrow from turning stem cells into essential cells. Leukemia, Hodgkin's disease, and other lymphoma cancers are known to damage the marrow's productive ability and destroy stem cells.
The leading treatment for conditions that threaten bone marrow's ability to function is a bone marrow transplant. A bone marrow transplant is used to rebuild the body's capacity to produce blood cells and bring their numbers to normal levels. Illnesses that may be treated with a bone marrow transplant include both cancerous and noncancerous diseases.
Cancerous diseases may or may not specifically involve blood cells, but cancer treatment can destroy the body's ability to manufacture new blood cells.
This procedure typically begins with chemotherapy to eliminate the compromised marrow. A matching donor must then be found; in most cases, this is a close family member.
Types of bone marrow transplant
Types of bone marrow transplant include:
- Autologous transplant: patients receive their own stem cells
- Syngeneic transplant: patients receive stem cells from their identical twin
- Allogeneic transplant: patients receive matching stem cells from their brother, sister, or parent or an unrelated donor
- Haploidentical transplantation: a treatment option for the approximately 70% of patients who do not have an HLA-identical matching donor
- Umbilical cord blood: a type of allogeneic transplant. Stem cells are removed from a newborn baby's umbilical cord right after birth. The stem cells are frozen and stored until they are needed for a transplant. Umbilical cord blood cells are very immature so there is less of a need for matching, but blood counts take much longer to recover.
Tissue type
Tissue type, also known as human leukocyte antigens (HLA) type, helps the body fight infection. To check if the tissue type is compatible, doctors check how many proteins on the surface of the blood cells match. There are millions of different tissue types but some are more common than others.
Tissue type is inherited, with these types being passed on from each parent. This means a relative will be more likely to have a matching tissue type. However, if a suitable bone marrow donor cannot be found from family members, doctors will try to find someone with a compatible tissue type on the bone marrow donor register.
Reasons for bone marrow transplants
The list of diseases for which HSCT is being used is rapidly increasing. More than half of autologous transplantations are performed for multiple myeloma and non-Hodgkin lymphoma, and a vast majority of allogeneic transplants are performed for hematologic and lymphoid cancers.
Every 4 minutes in the US, someone is diagnosed with a blood cancer. For many patients, a bone marrow transplant is the best chance for survival. While 30% of patients can find a matching donor in their families, 70% - approximately 14,000 each year - must rely on unrelated donations.
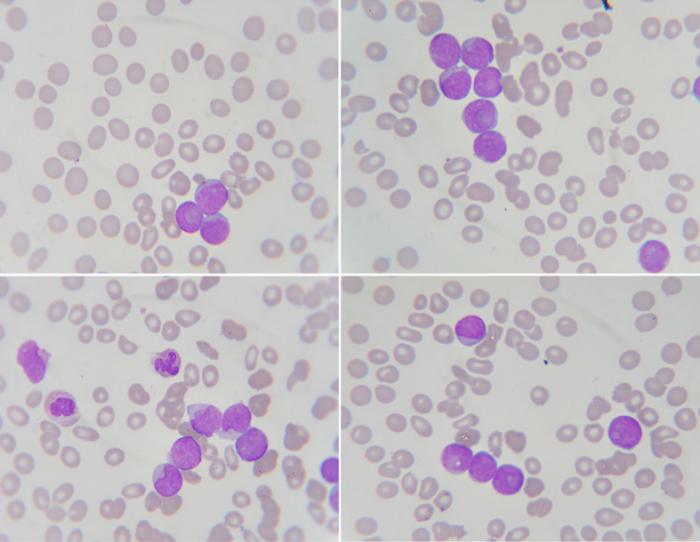
Blood smear showing neutrophil, white blood cell and leukemia.
Autologous HSCT is used to treat the following conditions:
- Multiple myeloma
- Non-Hodgkin lymphoma
- Hodgkin lymphoma
- Acute myeloid leukemia
- Neuroblastoma
- Germ cell tumors
- Autoimmune disorders (systemic lupus erythematosus, systemic sclerosis)
- Amyloidosis.
Allogeneic HSCT is used to treat the following disorders:
- Acute myeloid leukemia
- Acute lymphoblastic leukemia
- Chronic myeloid leukemia
- Chronic lymphocytic leukemia
- Myeloproliferative disorders
- Myelodysplastic syndromes
- Multiple myeloma
- Non-Hodgkin lymphoma
- Hodgkin lymphoma
- Aplastic anemia
- Pure red cell aplasia
- Paroxysmal nocturnal hemoglobinuria
- Fanconi anemia
- Thalassemia major
- Sickle cell anemia
- Severe combined immunodeficiency
- Wiskott-Aldrich syndrome
- Hemophagocytic lymphohistiocytosis
- Inborn errors of metabolism - E.g., mucopolysaccharidosis
- Gaucher disease, metachromatic leukodystrophies and adrenoleukodystrophies
- Epidermolysis bullosa
- Severe congenital neutropenia
- Shwachman-Diamond syndrome
- Diamond-Blackfan anemia
- Leukocyte adhesion deficiency.
HSCT may also be effective in the treatment of the following conditions:17
- Breast cancer - HSCT in breast cancer patients is debatable.
- Testicular cancer - The achievement of disease-free survival in a minority of patients with severe disease suggests much better results if performed earlier.
- Thalassemia - An 80% disease-free survival rate is achieved after allogeneic HSCT.
- Sickle cell anemia - Sickle cell anemia is potentially curable with allogeneic HSCT.
- Genetic disorders - Many genetic immunologic or hematopoietic disorders are potentially curable with allogeneic HSCT.
Bone marrow transplants are also sometimes necessary following certain treatments, such as high-dose chemotherapy and radiation therapy, which are often used to treat cancer. These treatments tend to damage healthy stem cells as well as destroying cancer cells.
Diagnosis and preparation
Several tests are performed before the bone marrow transplant, to identify any potential problems. Tests include:
- Tissue typing and a variety of blood tests
- Chest X-ray
- Pulmonary function tests
- Computed tomography scan (CT or CAT scan)
- Heart function tests including an electrocardiogram and echocardiogram
- Bone marrow biopsy
- Skeletal survey.
In addition, a complete dental exam is needed, before bone marrow transplant, to reduce the risk of infection. Other precautions will also be conducted before the transplant to reduce the patient's risk of infection.
How is bone marrow harvested?
Bone marrow can be obtained for examination by bone marrow biopsy and bone marrow aspiration. Bone marrow harvesting has become a relatively routine procedure and is generally aspirated from the posterior iliac crests while the donor is under either regional or general anesthesia.17
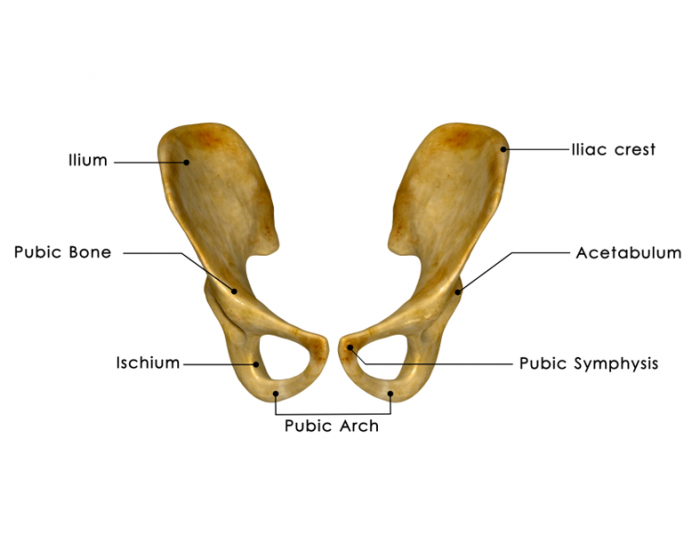
Red marrow has the strongest concentrations in the bones of the hips (ilium). The doctor will insert a needle into the bone and withdraw some of the bone marrow, which is then stored and frozen.
The sternum can also be used as an aspiration site and in children; the upper tibia can provide a good sample because it still contains a substantial amount of red bone marrow. The average number of cells in a leg bone is about 440 billion.
The doctor will insert a needle into the bone - usually in the hip - and withdraw some of the bone marrow, which is then stored and frozen.
Guidelines established by the National Marrow Donor Program (NMDP) limit the volume of bone marrow removed to 15 mL/kg of donor weight.
A dose of 1 X 108 and 2 X 108 marrow mononuclear cells per kilogram are required to establish engraftment in autologous and allogeneic marrow transplants, respectively.
Complications related to bone marrow harvesting are rare and involve anesthetic, infectious and bleeding problems.
Another option for evaluating bone marrow function is to administer certain drugs that stimulate the release of stem cells from the bone marrow into circulating blood. The blood sample is then obtained, and stem cells are isolated for microscopic examination. In newborns, stem cells may be retrieved from the umbilical cord.
How does a bone marrow transplant occur?
Before the transplant, chemotherapy, radiation, or both may be given. This may be done in two ways:
- Ablative (myeloablative) treatment: high-dose chemotherapy, radiation, or both are given to kill any cancer cells. This also kills all healthy bone marrow that remains, and allows new stem cells to grow in the bone marrow
- Reduced intensity treatment, also called a mini transplant: patients receive lower doses of chemotherapy and radiation before a transplant, which allows older patients, and those with other health problems to have a transplant.
A stem cell transplant is usually done after chemotherapy and radiation are complete.
The infusion of either bone marrow or peripheral blood is a relatively simple process that is performed at the bedside. The bone marrow product is infused through a central vein through an IV tube over a period of several hours. Autologous products are almost always cryopreserved; they are thawed at the bedside and infused rapidly over a period of several minutes.17

Bone marrow product is infused through a central vein through an IV tube over a period of several hours.
After entering the bloodstream, the hematopoietic stem cells travel to the bone marrow, where they begin to produce new white blood cells, red blood cells and platelets in a process known as "engraftment." Engraftment usually occurs within about 2 to 4 weeks after transplantation.4
Minimal toxicity has been observed in most cases. ABO-mismatched bone marrow infusions could occasionally lead to hemolytic reactions.
Dimethyl sulfoxide (DMSO), which is used for the cryopreservation of stem cells, may give rise to facial flushing, tickling sensation in the throat, and a strong taste in the mouth (the taste of garlic).
Rarely, it could cause bradycardia, abdominal pain, encephalopathy/seizures and renal failure. To avoid the risk of encephalopathy, which occurs with doses above 2 g/kg/day of DMSO, stem cell infusions exceeding 500 mL are infused over 2 days and the rate of infusion is limited to 20 mL/min.
Doctors check blood counts on a frequent basis. Complete recovery of immune function takes up to several months for autologous transplant recipients and 1 to 2 years for patients receiving allogeneic or syngeneic transplants.
Doctors evaluate the results of various blood tests to confirm that new blood cells are being produced and that the cancer has not returned. Bone marrow aspiration can also help doctors determine how well the new marrow is working.4
What are the risks of bone marrow transplants?
Complications associated with HSCT include both early and late effects.17
Early-onset problems include the following:
- Mucositis
- Hemorrhagic cystitis
- Prolonged, severe pancytopenia
- Infection
- GVHD
- Graft failure
- Pulmonary complications
- Hepatic veno-occlusive disease
- Thrombotic microangiopathy.
Late-onset problems include the following:
- Chronic GVHD
- Ocular effects
- Endocrine effects
- Pulmonary effects
- Musculoskeletal effects
- Neurologic effects
- Immune effects
- Infection
- Congestive heart failure
- Subsequent malignancy.
Major risks associated with bone marrow transplant include increased susceptibility to infection, anemia, graft failure, respiratory distress, and excess fluid, which can lead to pneumonia and liver dysfunction. In addition, a mismatch between donor and recipient tissues can lead to an immune reaction between cells of the host and cells of the graft.
When graft cells attack host cells, the result is a dangerous condition called graft-versus-host disease (GVHD), which may be acute or chronic and may manifest as a skin rash, gastrointestinal illness, or liver disease. The risk of GVHD can be minimized through careful tissue matching.
However, even when a donor antigen match is identical, roughly 40% of recipients still develop GVHD. This figure increases to between 60-80% when only a single antigen is mismatched. Because of the danger of this complication, autologous transplants are more commonly performed.
Bone marrow transplantation initially was not recommended for patients over age 50, because of higher mortality and morbidity results and because the incidence of GVHD increases in those over age 30. However, many transplant centers have performed successful bone marrow transplantations in patients well beyond age 50. People who donate bone marrow incur no risk because they generate new marrow to replace that which has been removed.
What is bone marrow donation?
There are two main types of bone marrow donation. The first is a bone marrow donation which involves the removal of bone marrow from the back of the pelvic bone.
It is blood stem cells, rather than the bone marrow itself, which are necessary for the treatment of blood cancers and other diseases.
The second, peripheral blood stem cell (PBSC) donation, is the more common method and involves filtering stem cells directly from the blood. It is these blood stem cells, rather than the bone marrow itself, which are necessary for the treatment of blood cancers and other diseases.
When an individual joins a bone marrow donation registry, they are agreeing to donate using whichever method the patient's doctor deems appropriate.
In terms of costs, the expense of making a blood marrow donation is usually covered by either the NMDP or the patient's medical insurance. Donors never pay for donating, and are never paid to donate.
In terms of risk, the dangers involved in the bone marrow donation process are minimal. Over 99% of donors make a full recovery after the procedure. With blood marrow donation, the major risk involves the use of anesthesia during the procedure itself.
With PBSC donation, the risks are minimal. The procedure itself, which involves filtering blood through a machine, is not considered dangerous.
A patient's likelihood of finding a donor that will give them bone marrow ranges from 66%-93%, depending on race or ethnicity. The likelihood of finding a donor is estimated at:
- 66% for African-American patients
- 72% for Hispanic or Latino patients
- 73% for Asian and Pacific Islander patients
- 82% for American Indian and Alaska Native patients
- 93% for White patients.
Who can donate bone marrow8
The following are some general guidelines for bone marrow donation as recommended by the NMDP. These guidelines are put into place to protect the health and safety of the donor and the recipient. Donors are encouraged to contact their local NMDP center for specific details and to discuss donations with their health care team.
- To be listed in the registry, potential donors must be healthy and between the ages of 18 and 60.
- If matched with a person needing a transplant, each donor must pass a medical examination and be infection-free before donating bone marrow.
- Most people taking medications can still donate bone marrow as long as they are healthy, and any medical conditions they have are under control at the time of the donation. Acceptable medications include birth control pills; thyroid medication; antihistamines; antibiotics; prescription eye drops; and topical medications, such as skin creams. Antianxiety and antidepressant drugs are allowed as long as the person's medical condition is under control.
- People who cannot donate bone marrow include pregnant women, users of intravenous drugs that are not prescribed by a doctor, people who have had a positive blood test for hepatitis B or hepatitis C, and those with specific medical conditions, such as most types of cancer or certain heart conditions.
- People with Lyme disease, malaria, or recent tattoos or piercings should wait at least a year before donating bone marrow.
How is a bone marrow match determined?
Once a person registers to donate, they will be asked to undertake an HLA-typing test, which is used to match up patients with potential donors. Their HLA type will then be added to a database of potential donors, which doctors can search through to find a match for their patients.
Once the HLA results are received, and are entered onto the registry of bone marrow donors, the potential donor will be contacted if they are matched to a patient.
A doctor will match their patient with a potential donor by comparing the proteins in blood cells to see if they are similar. The more similar they are, the better the chance of the patient's body accepting the transplant.
If the donor's tissue type matches that of a patient in need of a bone marrow transplant, they will be contacted.
Bone Marrow Donors Worldwide (BMDW) is a collective database of 59 registries in 43 countries, and 37 cord blood registries from 21 countries; 11,386,999 potential donors and cord units were available as of July 2007. Preliminary searches through the NMDP routinely also explore the BMDW.
What happens when donating bone marrow?
The following studies are routinely performed on hematopoietic stem cell donors:

Donating peripheral blood stem cells involves taking the blood using a catheter inserted in one arm, and passing the blood through a machine which filters out the stem cells.
- History and physical examination
- Serum creatinine, electrolyte, and liver function studies
- Serologic studies for cytomegalovirus (CMV), herpes viruses, HIV RNA, anti-HIV antibodies, hepatitis B and C viruses, human T-cell lymphotropic virus-1/2 (HTLV-I/II), and syphilis (VDRL); in autologous donations, CMV and VDRL testing are not required
- ABO blood typing
- HLA typing
- Chest radiography
- Electrocardiography (ECG).
Donating peripheral blood stem cells (PBSC)
Before a person can donate PBSC, they will need to undergo daily injections of a medication called filgrastim in the five days running up to the procedure. This medication draws stem cells from the bone marrow, so the donor will have more of them circulating in their blood.
Donating PBSC involves a procedure known as apheresis. This is when blood is taken from the body using a catheter inserted in one arm and passed through a machine, filtering out the stem cells, along with platelets and white blood cells. The remaining blood (consisting mainly of plasma and red blood cells) then flows back into the body through a vein in the other arm.
The procedure is completely painless and is similar to donating plasma. PBSC donation will usually require between 2 to 4 sessions, each between 2 to 6 hours.
PBSC donation does not require anesthesia. The medication that is given to stimulate the mobilization (release) of stem cells from the marrow into the bloodstream may cause bone and muscle aches, headaches, fatigue, nausea, vomiting or difficulty sleeping. These side effects usually stop within 2-3 days of the last dose of the medication.
Donating bone marrow
If a person is donating actual bone marrow instead of PBSC, the procedure will be entirely different. There will be no need for the filgrastim injections as the stem cells can be drawn directly from the bone marrow. Bone marrow donation is a surgical procedure, carried out in the operating room, which requires anesthesia and is completely painless. The entire procedure will only take between 1 and 2 hours.
In 96% of cases a general anesthetic will be used, which means the donator will be unconscious for the entire procedure. In a small number of cases a local anesthetic will be used, which simply numbs the area the bone marrow is taken from. In this situation, the person will be awake throughout the procedure.
The procedure occurs with the person lying on their stomach. The doctors will insert special, hollow needles into both sides of the pelvic bone, from which they will draw the liquid marrow. The incisions made by the needles will only be about a quarter of an inch in length and will not require stitches.
After the procedure, the person will be taken to a recovery room where they will stay until they have regained consciousness. Once they can eat, drink and walk, they will be able to leave.
Recovery
Once a donation is complete, it may take a couple of days to feel "normal", especially if surgery was involved. People who donate bone marrow often experience symptoms including headaches, fatigue, muscle pain, back or hip pain, bruising around the incision site and difficulty walking. These symptoms may last as little as a couple of days, or as long as several weeks.
For a person who donates PBSC, there is very little chance of any side effects following the donation, other than bruising at the needle site, and the recovery time is almost immediate.
After donation, bone marrow replaces itself within four to six weeks.
Outcomes
The outcome of bone marrow transplant depends on:
- The type of bone marrow transplant
- How well the donor's cells match the patient's
- What type of cancer or illness the patient has
- Age and overall health of the patient
- The type and dosage of chemotherapy or radiation therapy before transplant
- Any complications experienced.
In general, patients with stable disease or diseases in remission have better outcomes than those transplanted during a later disease phase or with relapsed disease. Young age at time of transplant also leads to more favorable outcomes.
Transplants for nonmalignant diseases generally have more favorable outcomes, with survival rate of 70-90% if the donor is a matched sibling, and 36-65% if the donor is unrelated. Transplants for acute leukemia in remission at the time of transplant have survival rates of 55-68% if the donor is related, and 26-50% if the donor is unrelated.
A bone marrow transplant may completely or partially cure illness. If the transplant is a success, individuals can go back to most normal activities as soon as they feel well enough. Usually, it can take up to 1 year to recover fully. Complications or failure of the bone marrow transplant can lead to death.
References:
1.
Encyclopedia
Britannica Bone marrow,
accessed 14 November 2014.
2.
Medscape Types of bone marrow,
last updated 22 August 2013, accessed 14 November 2014.
3.
Science Daily Reference article - bone marrow, accessed 14 November
2014.
4.
National Cancer
Institute Bone marrow transplantation and
peripheral blood stem cell transplantation, accessed 14 November
2014.
5.
John Hopkins Medicine Blood and bone marrow cancer
basics, accessed 14 November 2014.
6.
Society for Immunology Bone marrow,
accessed 14 November 2014.
7.
Explore Stem Cells Bone marrow stem cell harvest,
accessed 14 November 2014.
8.
Cancer.net Donating bone marrow,
accessed 14 November 2014.
9.
Centers for Disease
Control and Prevention (CDC) Stem cell (bone marrow) transplant, accessed 14
November 2014.
10.
Patient Stem cell transplant, last updated 15 October 2014,
accessed 14 November 2014.
11.
Myelodysplastic
Syndrome Foundation What does my bone marrow do? accessed
14 November.
12.
Surgery Encyclopedia Bone marrow transplantation,
accessed 14 November 2014.
13.
Medscape Blood cell formation,
updated 22 August 2013, accessed 14 November 2014.
14.
Macmillan The lymphatic system,
accessed 14 November 2014.
15.
Medscape Blood vessel barrier and
compartmentalization, updated 22 August 2013, accessed 14 November
2014.
16.
Delete Blood Cancer About blood cancer, accessed 14 November 2014.
17.
Medscape Hematopoietic stem cell transplantation, updated 31
March 2014, accessed 17 November 2014.
18.
Medscape Bone marrow anatomy – bone
marrow examination, updated 22 August 2013, accessed 17 November
2014.
19.
WebMD Bone marrow transplants and
stem cell transplants for cancer treatment, accessed 17 November
2014.
20.
Medscape Bone marrow transplantation –
the search process, updated 7 November 2014, access 17 November
2014.
21.
Medline Bone marrow transplant,
accessed 17 November 2014.
No comments:
Post a Comment