Parkinson's disease is a progressive nervous system disorder that affects how the person moves, including how they speak and write. Symptoms develop gradually, and may start off with ever-so-slight tremors in one hand.
Actor Michael J. Fox describes what it is like to have Parkinson's
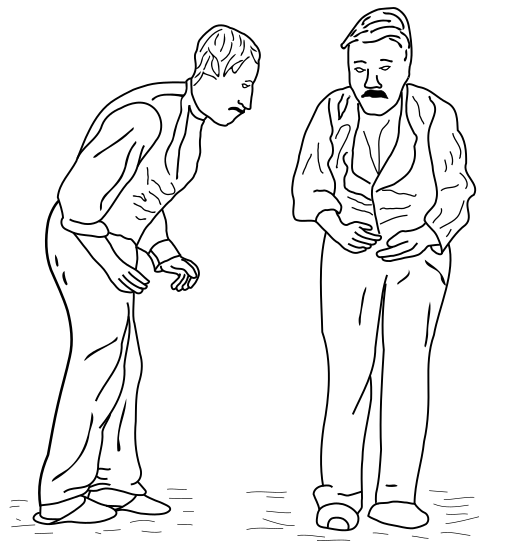
People with Parkinson's disease also experience stiffness and find they cannot carry out movements as rapidly as before - this is called bradykinesia. The muscles of a person with Parkinson's become weaker and the individual may assume an unusual posture.
Parkinson's disease belongs to a group of conditions called movement disorders. Movement disorders describe a variety of abnormal body movements that have a neurological basis, and include such conditions as cerebral palsy, ataxia, and Tourette syndrome.
Approximately one million adults in the USA are thought to live with Parkinson's disease; over 60,000 are diagnosed annually. The real figure is probably much higher when taking into account those who go undetected. According to the Parkinson's Disease Foundation, the economic toll of the disease in the USA is nearly $25 billion annually, including direct and indirect costs. The average annual medication costs for an American with Parkinson's disease is between $2,500 and $10,000.
In the United Kingdom approximately 127,000 people have Parkinson's disease - or 1 in every 500 people. About 10 million people around the world are estimated to be living with Parkinson's disease.
A male has a 50% higher risk of developing Parkinson's disease than a female.
In the majority of cases, symptoms start to appear after the age of 50. However, in about 4% to 5% of cases the sufferer is younger than 40 years. When signs and symptoms develop in an individual aged between 21 and 40 years, it is known as Young-onset Parkinson's disease.
Apart from tremor and slow movements, the patient may also have a fixed, inexpressive face - this is because of poorer control over facial muscle coordination and movement.
As a significant number of elderly patients with early Parkinson's disease symptoms assume that their traits may form part of normal aging and do not seek medical help, obtaining accurate statistics is probably impossible.
There are also several different conditions which sometimes have comparable signs and symptoms to Parkinson's, such as drug-induced Parkinsonism, head trauma, encephalitis, stroke, Lewy body dementia, corticobasal degeneration, multiple system atrophy, and progressive supranuclear pasly.
Parkinson's also affects the voice - a British mathematician believes he has created a cheap and easy to carry-out test using speech signal processing algorithms to accelerate the diagnosis of Parkinson's disease.
Max Little, who developed the algorithm at Oxford University, says that Parkinson's not only impacts on limb movement, but also on how people speak; on their voices.
Parkinson's also affects sense of smell - despite being incurable, doctors today can influence the course of the disease if Parkinson's is detected early enough; the destruction of brain cells can be slowed down - this means a better quality of life for the patient for many years. Scientists have recently discovered that hyposmia, losing one's sense of smell for no known cause, might be a marker for the non-motor signs of Parkinson's disease. The scientists said "Smelling tests in doctors' offices are suitable for detecting hyposmia, but so too are tests conducted in public places such as pedestrian zones."
Some factors may raise or lower the risk of developing Parkinson's
- Circumin - an ingredient found in the spice turmeric, is apparently effective in preventing the clumping of a protein involved in Parkinson's disease, according to scientists from Michigan State University.
- Flavonoids - adult males who regularly eat foods rich in flavonoids appear to have a considerably lower risk of developing Parkinson's disease, compared to others who do not, researchers in the USA and UK reported in the journal Neurology. Examples of foods include berries, apples, some vegetables, tea and red wine. In this study, the protective effects come from anthocyanins, a subclass of flavonoids.
- REM sleep disorder - people with REM (rapid eye movement) sleep behavior disorder may have twice the risk of developing Parkinson's disease or mild cognitive impairment, compared to others without the disorder, researchers at the Mayo Clinic reported in Annals of Neurology.
"Understanding that certain patients are at greater risk for MCI or Parkinson's disease will allow for early intervention, which is vital in the case of such disorders that destroy brain cells. Although we are still searching for effective treatments, our best chance of success is to identify and treat these disorders early, before cell death."
- Some reheated cooking oils - aldehydes, which have been linked to Parkinson's, Alzheimer's and other neurodegenerative diseases, as well as some cancers, can be found in some oils, such as sunflower oil, when heated to a certain temperature, and then used again. Scientists from the University of the Basque Country found that aldehydes remain in cooking oils after they are heated.
Parkinson's disease is primarily caused by low and falling dopamine levels
A person with Parkinson's has abnormally low dopamine levels. Dopamine-generating cells, known as dopaminergic neurons (types of nerve cells) in the substantia nigra part of the brain have died. Experts do not know why these cells die.When dopamine levels are too low, people find it harder to get things done, to control their movements.
Dopamine levels progressively drop in patients with the disease, so their symptoms gradually become more severe. Dopamine is involved in the sending of messages to the part of the brain that controls coordination and movement.

The substantia nigra is in the midbrain and plays an important role in movement, reward and addiction
- A chronic disease - a long-term disease. It is incurable.
- A progressive disease - a disease that gradually gets worse.
What is Parkinsonism?
Parkinsonism is a neurological syndrome characterized by tremor, rigidity, postural instability, and hypokinesia (decreased bodily movement).A syndrome is the association of several clinically recognizable features, signs, symptoms, phenomena or characteristics that often occur together.
Parkinson's disease is the most common cause of Parkinsonism. Put simply - Parkinsonism includes the signs and symptoms that resemble Parkinson's disease.
According to Medilexicon's medical dictionary, Parkinsonism is:
1. A neurologic syndrome usually resulting from deficiency of the neurotransmitter dopamine as the consequence of degenerative, vascular, or inflammatory changes in the basal ganglia; characterized by rhythmic muscular tremors, rigidity of movement, festination, droopy posture, and masklike facies.
2. A syndrome similar to parkinsonism. Some features seen with Parkinson's disease that occur with other disorders (progressive supranuclear palsy) or as a side effect of certain medications (antipsychotic drugs).
Parkinson's disease mentioned in history
Descriptions of people with Parkinsonism date back to ancient Egypt. It is also mentioned in the Christian Bible and Claudius Galenus' (Galen's) writings. Claudius Galenus (or Aelius Galenus), who lived from 129 AD to around 200 AD, was a well-known Roman (of Greek origin) doctor and philosopher.Then there seem to be no clear references to PD (Parkinson's Disease) until the 17th century. Auguste François Chomel, a French pathologist, John Hunter, a Scottish surgeon, Hieronymus David Gaubius, a German physician and chemist, and Franciscus Sylvius, a Dutch chemist, physiologist and anatomist, all described Parkinson's-type signs and symptoms during the 17th and 18th centuries.

James Parkinson
James Parkinson systematically described six people with signs and symptoms of the disease we know today as Parkinson's. They were not formally examined, but he observed them as they went on on their daily walks, and sometimes asked them to describe their symptoms to him. In his Essay Parkinson described the characteristic resting tremor, diminished muscle strength, paralysis, unusual posture and gait, and how the disease progresses over time.
Jean-Martin Charcot (1825-1893) - a French neurologist and professor of anatomical pathology, also known as the founder of modern neurology. His studies between 1868 and 1881 are described today by medical historians as a "landmark in the understanding of Parkinson's disease". He also clearly defined and explained the difference between rigidity, weakness and bradykinesia (a slowness in the execution of movement). Charcot is also famous for naming and being the first to describe multiple sclerosis.
Frederic Lewy (1885-1950) - a prominent American neurologist is best known for the discovery of Lewy bodies, characteristic indicators of Dementia with Lewy Bodies and Parkinson's disease.
Konstantin Nikolaevitch Tretiakoff (1892-1958) - a Russian neuropathologist. While writing his thesis for his doctorate at L'Assistance Publique des Hopitaux de Paris, France, he described the degeneration of the substantia nigra in cases of Parkinson's - he was the first to link this anatomic structure with Parkinson's disease. Tretiakoff's findings were not accepted by many in the medical community, until they were confirmed in further studies carried out by Rolf Hassler, in 1938.
Rolf Hassler (1914-1984) - a distinguished German pathologist. Hassler made important discoveries in the treatment of Parkinson's disease. In a 1938 published paper, he wrote that autopsies of Parkinson's patients showed that the most affected part of the brain was the substantia nigra pars pallidus, which lost many neurons and had an abundant accumulation of Lewy bodies. He became a pioneer in surgery for tremor.
Arvid Carlsson (1923) - a Swedish scientist who was awarded the Nobel Prize in Physiology/Medicine in 2000 for his work on dopamine, Carlsson is best known for his work with dopamine and its effects in Parkinson's disease. He demonstrated that dopamine is a neurotransmitter in the brain and not just a precursor for norepinephrine.
Carlsson and his research team at Astra AB (today AstraZeneca) managed to derive the first marketed SSRI (selective serotonin reuptake inhibitor) - zimelidine - from brompheniramine. He noticed that dopamine levels in the basal ganglia are particularly high - this part of the brain is important for movement. He then demonstrated that when animals were given reserpine, a drug, dopamine levels dropped and the animals lost movement control - he explained that in Parkinson's disease, dopamine levels also fall, causing loss of movement.
Carlsson then showed that when L-Dopa was administered to the animals, their symptoms were alleviated. L-Dopa is a precursor of dopamine. This breakthrough led doctors to try L-Dopa on their Parkinson's patients with early symptoms. L-Dopa is still the basis for most drugs prescribed for Parkinson's disease symptoms.
Kazimierz Funk (anglicized as Casimir Funk 1884 - 1967) - a Polish biochemist. Until the arrival of "levodopa", anticholinergics and surgery were the only available treatments for patients with Parkinson's. Funk first synthesized levodopa (L-Dopa) in 1911, but it was not until the middle of the last century that it received any attention. In 1967, levodopa entered clinical practice and revolutionized Parkinson's management.
Does a good night's sleep help Parkinson's patient's motor function?
Dutch researchers recently found that Parkinson's patients say their motor function is better in the mornings if they had a good night's sleep. This is surprising, because they wake up after several hours on no medication.The researchers, who published their study in the Journal of Parkinson's Disease, say that the phenomenon of sleep benefit has been studied for several years, but no consistent variables have been found.
References:

No comments:
Post a Comment